Madaxweyne Donald Trump ayaa amray in ciidamada Mareykan ah loo diro magaalada Portland ee gobolka…
Why Vaccinated People Are Getting ‘Breakthrough’ Infections
By Apoorva Mandavilli, New York Times
A wedding in Oklahoma leads to 15 vaccinated guests becoming infected with the coronavirus. Raucous Fourth of July celebrations disperse the virus from Provincetown, Mass., to dozens of places across the country, sometimes carried by fully vaccinated celebrants.
As the Delta variant surges across the nation, reports of infections in vaccinated people have become increasingly frequent — including, most recently, among at least six Texas Democrats, a White House aide and an aide to Speaker Nancy Pelosi.
The highly contagious variant, combined with a lagging vaccination campaign and the near absence of preventive restrictions, is fueling a rapid rise in cases in all states, and hospitalizations in nearly all of them. It now accounts for about 83 percent of infections diagnosed in the United States.
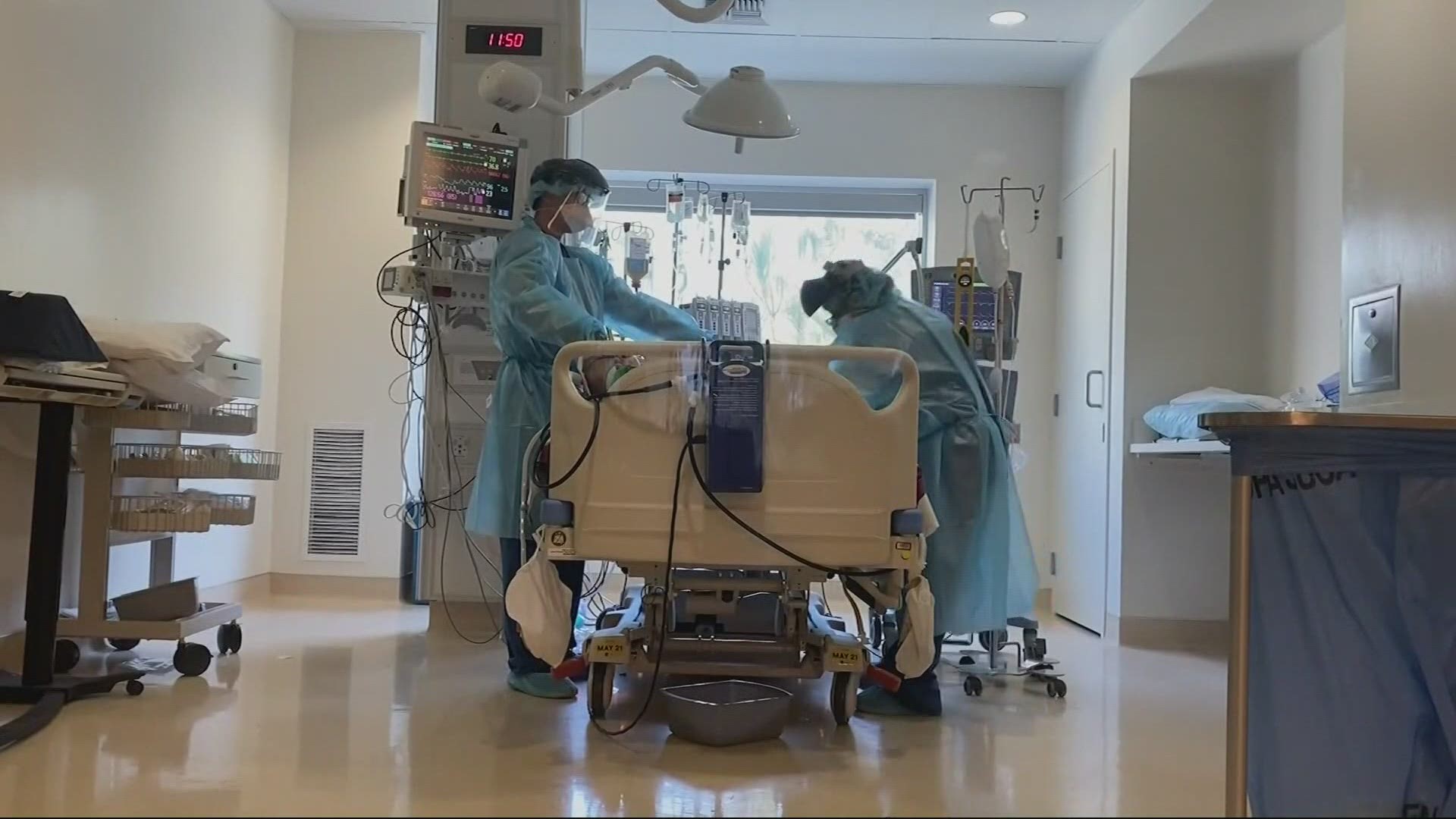
But as worrying as the trend may seem, breakthrough infections — those occurring in vaccinated people — are still relatively uncommon, experts said, and those that cause serious illness, hospitalization or death even more so. More than 97 percent of people hospitalized for Covid-19 are unvaccinated.
“The takeaway message remains, if you’re vaccinated, you are protected,” said Dr. Celine Gounder, an infectious disease specialist at Bellevue Hospital Center in New York. “You are not going to end up with severe disease, hospitalization or death.”
Reports of breakthrough infections should not be taken to mean that the vaccines do not work, Dr. Anthony S. Fauci, the Biden administration’s top pandemic adviser, said on Thursday at a news briefing.
“By no means does that mean that you’re dealing with an unsuccessful vaccine,” he said. “The success of the vaccine is based on the prevention of illness.
Still, vaccinated people can come down with infections, overwhelmingly asymptomatic or mild. That may come as a surprise to many vaccinated Americans, who often assume that they are completely shielded from the virus. And breakthrough infections raise the possibility, as yet unresolved, that vaccinated people may spread the virus to others.
Given the upwelling of virus across much of the country, some scientists say it is time for vaccinated people to consider wearing masks indoors and in crowded spaces like shopping malls or concert halls — a recommendation that goes beyond current guidelines from the Centers for Disease Control and Prevention, which recommends masking only for unvaccinated people.
The agency does not plan to change its guidelines unless there is a significant change in the science, said a federal official speaking on condition of anonymity because he was not authorized to speak on the matter.
The agency’s guidance already gives local leaders latitude to adjust their policies based on rates of transmission in their communities, he added. Citing the rise of the Delta variant, health officials in several California jurisdictions are already urging a return to indoor masking; Los Angeles County is requiring it.
“Seatbelts reduce risk, but we still need to drive carefully,” said Dr. Scott Dryden-Peterson, an infectious disease physician and epidemiologist at Brigham & Women’s Hospital in Boston. “We’re still trying to figure out what is ‘drive carefully’ in the Delta era, and what we should be doing.”
The uncertainty about Delta results in part from how it differs from previous versions of the coronavirus. Although its mode of transmission is the same — it is inhaled, usually in indoor spaces — Delta is thought to be about twice as contagious as the original virus.
Significantly, early evidence also suggests that people infected with the Delta variant may carry roughly a thousandfold more virus than those infected with the original virus. While that does not seem to mean that they get sicker, it does probably mean that they are more contagious and for longer.
Dose also matters: A vaccinated person exposed to a low dose of the coronavirus may never become infected, or not noticeably so. A vaccinated person exposed to extremely high viral loads of the Delta variant is more likely to find his or her immune defenses overwhelmed.
The problem grows worse as community transmission rates rise, because exposures in dose and number will increase. Vaccination rates in the country have stalled, with less than half of Americans fully immunized, giving the virus plenty of room to spread.
Unvaccinated people “are not, for the most part, taking precautions, and that’s what’s driving it for everybody,” said Dr. Eric J. Rubin, the editor in chief of the New England Journal of Medicine. “We’re all susceptible to whatever anyone’s behavior is in this epidemic.”
Dr. Gounder likened the amount of protection offered by the vaccines to a golf umbrella that keeps people dry in a rainstorm. “But if you’re out in a hurricane, you’re still going to get wet,” she said. “That’s kind of the situation that the Delta variant has created, where there’s still a lot of community spread.”
For the average vaccinated person, a breakthrough infection is likely to be inconsequential, causing few to no symptoms. But there is concern among scientists that a few vaccinated people who become infected may go on to develop long Covid, a poorly understood constellation of symptoms that persists after the active infection is resolved.

Much has been made of Delta’s ability to sidestep immune defenses. In fact, all of the existing vaccines seem able to prevent serious illness and death from the variant. In laboratory studies, Delta actually has proved to be a milder threat than Beta, the variant first identified in South Africa.
Whether a vaccinated person ever becomes infected may depend on how high antibodies spiked after vaccination, how potent those antibodies are against the variant, and whether the level of antibodies in the person’s blood has waned since immunization.
In any case, immune defenses primed by the vaccines should recognize the virus soon after infection and destroy it before significant damage occurs.
“That is what explains why people do get infected and why people don’t get seriously ill,” said Michel C. Nussenzweig, an immunologist at Rockefeller University in New York. “It’s nearly unavoidable, unless you’re going to give people very frequent boosters.”
Understand the State of Vaccine Mandates in the U.S.
-
- College and universities. More than 400 colleges and universities are requiring students to be vaccinated for Covid-19. Almost all are in states that voted for President Biden.
- Hospitals and medical centers. Many hospitals and major health systems are requiring employees to get the Covid-19 vaccine, citing rising caseloads fueled by the Delta variant and stubbornly low vaccination rates in their communities, even within their work force. In N.Y.C., workers in city-run hospitals and health clinics will be required to get vaccinated or else get tested on a weekly basis.
- Federal employees. President Biden will formally announce on Thursday that all civilian federal employees must be vaccinated against the coronavirus or be forced to submit to regular testing, social distancing, mask requirements and restrictions on most travel. State workers in New York will face similar restrictions.
- Can your employer require a vaccine? Companies can require workers entering the workplace to be vaccinated against the coronavirus, according to recent U.S. government guidance.
There is limited evidence beyond anecdotal reports to indicate whether breakthrough infections with the Delta variant are more common or more likely to fan out to other people. The C.D.C. has recorded about 5,500 hospitalizations and deaths in vaccinated people, but it is not tracking milder breakthrough infections.
Additional data is emerging from the Covid-19 Sports and Society Workgroup, a coalition of professional sports leagues that is working closely with the C.D.C. Sports teams in the group are testing more than 10,000 people at least daily and sequencing all infections, according to Dr. Robby Sikka, a physician who worked with the N.B.A.’s Minnesota Timberwolves.
Breakthrough infections in the leagues seem to be more common with the Delta variant than with Alpha, the variant first identified in Britain, he said. As would be predicted, the vaccines cut down the severity and duration of illness significantly, with players returning less than two weeks after becoming infected, compared with nearly three weeks earlier in the pandemic.
But while they are infected, the players carry very high amounts of virus for seven to 10 days, compared with two or three days in those infected with Alpha, Dr. Sikka said. Infected players are required to quarantine, so the project has not been able to track whether they spread the virus to others — but it’s likely that they would, he added.
“If they’re put just willy-nilly back into society, I think you’re going to have spread from vaccinated individuals,” he added. “They don’t even recognize they have Covid because they think they’re vaccinated.”
Elyse Freitas was shocked to discover that 15 vaccinated people became infected at her wedding. Dr. Freitas, 34, a biologist at the University of Oklahoma, said she had been very cautious throughout the pandemic, and had already postponed her wedding once. But after much deliberation, she celebrated the wedding indoors on July 10.
Based on the symptoms, Dr. Freitas believes that the initial infection was at a bachelorette party two days before the wedding, when a dozen vaccinated people went unmasked to bars in downtown Oklahoma City; seven of them later tested positive. Eventually, 17 guests at the wedding became infected, nearly all with mild symptoms.
“In hindsight, I should have paid more attention to the vaccination rates in Oklahoma and the emergence of the Delta variant and adjusted my plans accordingly,” she said.

An outbreak in Provincetown, Mass., illustrates how quickly a cluster can grow, given the right conditions. During its famed Fourth of July celebrations, the small town hosted more than 60,000 unmasked revelers, dancing and mingling in crowded bars and house parties.
The crowds this year were much larger than usual, said Adam Hunt, 55, an advertising executive who has lived in Provincetown part time for about 20 years. But the bars and clubs didn’t open until they were allowed to, Mr. Hunt noted: “We thought we were doing the right thing. We thought we were OK.”
Mr. Hunt did not become infected with the virus, but several of his vaccinated friends who had flown in from places as far as Hawaii and Alabama tested positive after their return. In all, the cluster has grown to at least 256 cases — including 66 visitors from other states — about two-thirds in vaccinated people.
“I did not expect that people who were vaccinated would be becoming positive at the rate that they were,” said Steve Katsurinis, chair of the Provincetown Board of Health. Provincetown has moved swiftly to contain the outbreak, reinstating a mask advisory and stepping up testing. It is conducting 250 tests a day, compared with about eight a day before July 1, Mr. Katsurinis said.
Health officials should also help the public understand that vaccines are doing what they are supposed to — preventing people from getting seriously ill, said Kristen Panthagani, a geneticist at Baylor College of Medicine who runs a blog explaining complex scientific concepts.
“Vaccine efficacy isn’t 100 percent — it never is,” she said. “We shouldn’t expect Covid vaccines to be perfect, either. That’s too high an expectation.”
SOURCE: New York Times


